Tooth decay - Treatment for decayed teeth
Dental caries is one of the most common chronic diseases of the oral cavity, found in all age groups, with a global incidence that continues to increase, despite advances in the field of prophylaxis and dental treatments. The process of caries development affects teeth through a complex biological mechanism involving the action of bacteria, the presence of carbohydrates and the imbalance between demineralization and remineralization. The evolution of caries is influenced by numerous factors, from poor oral hygiene, a diet rich in sugars and lack of fluoridation, to the morphological peculiarities of the teeth and the individual characteristics of the salivary composition.
What are dental caries?
Dental caries is a disease of the dental tissues, of an infectious nature, with a progressive nature, which affects the hard structures of the tooth: enamel, dentin and, in advanced forms, the root cementum. Cavities develop as a result of the growth of bacteria that live in the oral cavity and that break down food debris left after a meal, producing acids. Acids lower the pH of the mouth, and when the decrease approaches the threshold of 5.5, the tooth enamel begins to be affected. From this point, the cavity can progress if not treated properly, affecting the interior of the tooth, reaching the pulp and nerve, in which case pain begins to appear. It is important to attend annual dental check-ups to keep a close eye on the development of incipient cavities.
Why do dental cavities occur - The main causes
The development of dental cavities involves a combination of factors, from biological aspects to behavioral and environmental factors. The main causes of dental cavities include:
- oral microflora - bacteria that live in the oral cavity involved in lowering the local pH and producing organic acids;
- frequent consumption of sugars and carbohydrates (such as sweet snacks between meals)
- poor oral hygiene;
- reduced or qualitatively altered salivary flow;
- poorly mineralized tooth structure;
- frequency and consistency of meals (frequent sweet snacks between meals contribute significantly to the development of caries);
- socio-economic factors: reduced access to dental services, low level of health education, unbalanced diet;
- genetic predispositions regarding salivary composition, enamel structure and dental eruptive pattern.
Symptoms of dental caries
Manifestations of dental caries depend on the depth of the lesion and the degree of damage to hard tissues. In the early stages, symptoms may be absent or minimal, while in advanced forms spontaneous pain and septic complications appear. Common symptoms include:
- discoloration of the enamel;
- dental sensitivity to thermal (cold, hot) or osmotic (sweet, sour) stimuli;
- intermittent or continuous pain, localized or irradiated, occurring during mastication or spontaneously;
- persistent halitosis (bad smell from the oral cavity), generated by the accumulation of food debris and anaerobic bacterial activity in the carious cavity;
- localized gingival or periodontal edema;
- fistula with suppuration.
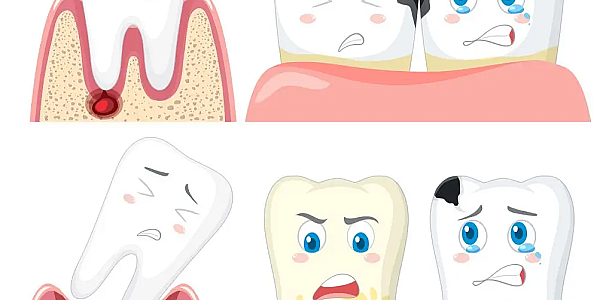
Types of tooth decay depending on location
Dental caries can occur in different areas of the oral cavity, but also in certain areas of the teeth, these particularities allowing to understand how the lesions affect the dental structures according to the anatomical area involved. Each type of location presents particular clinical and evolutionary characteristics, which determine an appropriate treatment approach.
Coronal caries or caries on the contact surface (occlusal, interdental, cervical)
Coronal caries affect the visible portion of the tooth, more precisely the crown, the one that we can see and care for easily. Coronal caries or caries on the contact surface are the most common and are divided, depending on the specific area, into occlusal, interdental and cervical caries. Occlusal caries occurs on the contact surface of molars and premolars, in the grooves and depressions of the teeth that favor the appearance of bacterial plaque. Interdental caries develops between the teeth, in the adjacent contact points, where the access of the toothbrush is limited. Cervical caries occurs in the area of the enamel-cement junction, that is, in the area where the enamel meets the root and where again bacterial plaque can easily appear.
Root Caries
Root caries affects the root surface of the teeth and is found especially in elderly patients, with gingival retraction (retreat of the gums) and exposure of the root cementum. Cementum does not have the same resistance as enamel and for this reason is extremely vulnerable to the general acid from the decomposition of food debris as a result of the action of bacteria in the mouth. Beneath this layer is dentin, which can allow bacteria to reach the nerve of the tooth. The causes that lead to the appearance of root caries are: dry mouth, poor oral hygiene, unsuitable dentures and a diet rich in sugars.
Caries on the lateral surfaces of the tooth
Caries that appear on the lateral parts of the teeth, such as the area towards the cheek or palate, are due either to incorrect brushing or the use of unsuitable care products. Although the area is easier to brush, if the toothbrush is too hard or the toothpaste too abrasive, these things can lead to the accentuation of incipient cavities. Brushing must be done correctly in this area, taking care not to be too aggressive.
Secondary cavities
Secondary cavities occur around existing fillings, either due to structural changes that have occurred over time or because the filling is not suitable. This type of cavity can lead to damage to the fillings, but also to the continued evolution of cavities on a restored tooth.
Types of dental caries by stage
Caries can also be classified according to the severity of the situation, more precisely how deep it is in the tooth structure. Usually, the classification includes three stages: superficial, medium and deep. The delimitation between a superficial, medium or deep caries is clinically relevant, as it defines both the severity of the pathological process and the type of intervention required.
Superficial dental caries
Superficial dental caries are limited to the enamel layer and represent the incipient form of dental caries. At this stage we are only talking about the loss of mineral substance from the enamel, but the caries is not visible in the form of a cavity, but only in the form of opaque white spots, smooth to the touch. At this stage, there is no deep bacterial invasion and no perceptible symptoms appear, which is why the diagnosis is frequently established during a routine dental consultation.
Medium Tooth Decay
Medium tooth decay involves both the enamel and the outer dentin, with visible structural damage and possible sensitivity to external stimuli. Specifically, you can tell that you have a cavity when you experience sensitivity to sweet or cold, or even when pressing on the tooth. Because the bacteria reach the dentin, the nerve becomes irritated, and this is where the sensation of pain occurs.
Deep tooth decay
Deep tooth decay affects the inner dentin, approaching the pulp chamber, which increases the risk of irreversible damage to the pulp. At this stage, the bacteria can cause acute pulp inflammation, which is clinically manifested by intense, throbbing pain, which occurs especially at night.
Decayed Teeth in Children
Dental caries in children develops at an accelerated rate due to the characteristics of temporary teeth. The risk increases significantly in the presence of predisposing factors, such as a diet rich in sugars, inadequate oral hygiene, lack of regular dental check-ups and the transmission of bacteria through contaminated utensils. The most common forms of caries in children include bottle-feeding caries, rampant caries and interproximal lesions in temporary molars.

Developmental stages of dental caries
Dental caries evolves in a predictable way, going through a sequence of stages that reflect the progression from the enamel to the deep tissues of the tooth. Identifying the exact moment when the lesion can be stopped or reversed is very important for preserving teeth and preventing complications. The stages of evolution include: enamel demineralization, incipient caries (with the appearance of a cavity), medium caries (bacteria affect the dentin), pulp damage and, finally, dental abscess. The rate of evolution varies depending on the type and frequency of food, salivary composition, oral hygiene, enamel density and the presence of fluoride.
Enamel demineralization
Demineralization represents the onset of the caries process, characterized by the loss of minerals from the enamel and the decrease in the pH of the mouth as a result of the decomposition of food debris by bacteria. As a result, opaque white spots with diffuse edges begin to appear on the teeth, a sign that there is a cavity there that requires treatment.
Early caries
The early stage of caries is characterized by the appearance of a minimal cavity, limited to the enamel or superficially touching the dentin. The enamel becomes brittle, fractures under the pressure of chewing, and bacteria penetrate the dentin layer, where propagation is accelerated by the increased porosity of the tooth (as a result of the loss of enamel and minerals). Although symptoms are rare or absent, some patients may complain of sensitivity to sweet or cold.
Medium caries
When the caries reaches the dentin, but not the pulp chamber, we are talking about medium caries. The inflammation that occurs as a result of this process causes pain and irritation of the dental nerve.
Damage to the dental pulp
Once the pulp chamber is reached, bacteria induce acute or chronic inflammation. Blood vessels dilate, and the immune system begins to fight the inflammation. The pain becomes intense, throbbing, often at night, and may be associated with increased sensitivity to cold or sweet.
Tooth abscess
The final stage of untreated tooth decay is the formation of a dental abscess, a pocket of pus around the root of the tooth. Left untreated, the infection can spread to the tissues and bone of the tooth, or even throughout the body. Symptoms of a tooth abscess can include fever, pain, and swollen glands as the immune system tries to fight the infection.
How do you recognize early-stage caries?
Early identification of dental caries is an important objective in dentistry, as it allows for minimally invasive treatments and the maintenance of dental vitality. In the early stage, the lesion is limited to the enamel layer, without dentinal damage and without the presence of a cavity detectable upon palpation. Clinical signs are discreet but characteristic. Most commonly, an opaque white area appears, smooth to the touch, with a matte appearance, located especially on the occlusal surfaces of the molars or in the interdental areas.
When should you see a doctor?
A dental consultation becomes necessary when signs appear that may indicate the onset or progression of dental caries. The presence of pigmented spots, changes in color on the tooth surface, sensitivity to cold, sweet or pressure, spontaneous pain or when chewing, are indications that justify immediate dental check-up.
Treatment for dental caries
The treatment of dental caries is determined depending on the location of the caries, its depth and the degree of damage to the tooth. In the early stages, the application of fluoride can stop the development of caries. In the middle stages, filling with composite materials is recommended. Deep lesions often require endodontic treatment, and in case of severe coronal destruction, prosthetic restoration or restorative odontherapy is recommended. In terminal situations, tooth extraction becomes inevitable.
Dental filling
Dental filling with fillings is indicated at the stage in which the tooth has cavities (holes), when the enamel structure is destroyed, with the formation of a clinically visible and palpable void. Filling involves the removal of carious tissue and the restoration of the dental crown with photopolymerizable composite materials or ionomers. The application is performed in layers, with biocompatible adhesives, to ensure the tightness of the cavity and prevent the recurrence of caries.
Dental crown
When the tooth is very damaged and the crown can no longer be saved, the restoration of the tooth is possible by applying a dental crown. Usually, the crown is recommended when more than half of the visible part of the tooth has been lost, a situation that often occurs in cases of deep cavities, loose fillings or fractures of the tooth.
Root canal treatment
Root canal treatment is the procedure by which infected or necrotic pulp tissue is removed from inside the tooth, followed by decontamination, shaping and obturation of the root canals. The indication for performing root canal treatment appears in the context of deep cavities, in which bacterial invasion reaches the pulp chamber and causes irreversible inflammation or tissue damage.
Tooth fluoridation
Professional fluoridation, like scaling, is an effective method of strengthening enamel and, implicitly, preventing cavities. During fluoridation, high-concentration fluoride gels or varnishes are used, applied periodically, especially in patients with a high risk of caries. Fluoride contributes to the formation of fluorapatite, with low solubility in acids.
Tooth extraction
Tooth extraction is required when the tooth has severe destruction, increased mobility or an infection that cannot be controlled. The intervention is performed under local anesthesia, and the area can subsequently be restored with an implant or a prosthetic bridge.
How much does treatment for dental caries cost?
Treatment costs vary depending on the complexity of the lesion, the materials used, the need for endodontic treatment and the prosthetic solutions chosen. A superficial caries is treated at low costs, while complex endodontic treatments or prosthetic restorations require higher investments.
Dental caries treatment - Price
| Procedure | Cost (in RON) |
| Superficial filling | 350 |
| Medium filling | 400 |
| Profound tooth filling | 450 |
| Temporary filling | 150 |
| Temporary crowns | between 50-300 |
| Metal-ceramic crown | 900 |
| Full ceramic crown | 1800 |
| Full zirconia crown | 1200 |
| Topical fluoridation in the office (both arches) | 200 |
| Tooth extraction | between 250-750 |
| Endodontic treatment with rotary instruments for monoradicular teeth / with microscope | 350 / 1000 |
| Endodontic treatment with rotary instruments for pluriradicular teeth / with microscope | 500 / 1300 |
Photo source: Freepik
Bibliography:
https://www.mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892
https://my.clevelandclinic.org/health/diseases/10946-cavities
https://medlineplus.gov/ency/article/001055.htm
https://www.cdc.gov/oral-health/about/cavities-tooth-decay.html
https://www.nhs.uk/conditions/tooth-decay
https://www.mayoclinic.org/diseases-conditions/cavities/diagnosis-treatment/drc-20352898
https://www.mchoralhealth.org/dental-sealant/3-tooth-selection/3-2.php
https://ameldental.com/en/dental-caries-types-causes-and-approaches-to-treatment
https://www.ncbi.nlm.nih.gov/books/NBK597361
https://www.researchgate.net/figure/Types-of-dental-caries-according-to-location-Type-A-caries-or-a-filling-on-the-crown_fig1_351300367
https://www.nidcr.nih.gov/health-info/tooth-decay/more-info/tooth-decay-process
Frequently asked questions about tooth decay

Dr. Nicoleta Taran answers questions: